LANCET COUNTDOWN ON HEALTH AND CLIMATE CHANGE
POLICY BRIEF FOR THE UNITED STATES OF AMERICA
OCTOBER 2021
This fifth annual Policy Brief is supported by a diverse group of health experts from over 70 institutions, organizations, and centers who recognize that climate change is first and foremost a health crisis. It uses indicator data for the United States (U.S.) from the 2021 global Lancet Countdown report1_ and recent scientific studies to expose the inequitable health risks of climate change and highlights opportunities to improve health through swift action. The U.S. must rapidly implement an all-encompassing, evidence-informed response to climate change that prioritizes and optimizes health and equity.
The state of climate change and health in the United States
Greenhouse gas (GHG) emissions, driven to a large extent by the burning of fossil fuels (e.g., coal, oil, and natural gas), have already warmed the world by 2°F (1.1°C) on average, compared to pre-industrial temperatures.2_ The long-predicted consequences of climate change are unfolding, and an urgent reduction in GHG emissions is required to try to avoid reaching 2.7°F (1.5°C) within the next two decades.2_
There is no safe global temperature rise from a health perspective, and additional warming will affect every U.S. region. Today’s adverse health impacts of climate change are varied and widespread (see past Briefs). All of us have been or likely will be affected by climate change, with some hazards more easily recognizable than others.1_ Climate change is worsening heat waves, amplifying droughts, intensifying wildfires, supercharging hurricanes, and fueling flood risk through increased heavy rainfall events and rising sea levels.2_ In 2020, a record-breaking 22 weather and climate disasters each caused over one billion dollars in damage (e.g., structural, crop) in the U.S. with over $95 billion dollars in total losses.3_ A record 11 hurricanes made landfall — seven as billion-dollar events.4_
Climate change can also produce less obvious harm. For example, climate change increases pollen levels that worsen allergic and respiratory conditions,5_ and climate-driven increases in temperature and precipitation make it easier to spread waterborne diseases that cause gastrointestinal illness.6_
While everyone’s health is already at risk, some populations bear a greater burden. Health risks from climate change escalate with increased exposure (e.g., by geography or type of work) and heightened susceptibility (e.g., with pregnancy, certain medical conditions, age). Decades of racially-biased policies have created inequities, placing individuals and communities who are Black, Latinx, Alaskan Native or American Indian, Asian American or Pacific Islander, and other people of color at increased risk (see 2020 Brief). Policies have also negatively impacted the health of low-income communities7_,8_ and made it harder to adapt to the rapidly changing climate. Proactive and timely adaptation can reduce risks.
This year’s Brief explores three interrelated hazards — extreme heat, droughts, and wildfires — to highlight the complexities and nuances of the impacts of climate change on health, including how health risks vary, can be unexpectedly broad, and have far-reaching consequences. It concludes by demonstrating how deepening this understanding is essential for evidence-informed policy recommendations. Specifically, it calls for policymakers to: 1) make urgent investments in research and interventions that protect health and prioritize equity, 2) account for the health costs of fossil fuel burning in decision-making, and 3) rapidly cut GHG emissions, particularly in areas suffering most from fossil fuel-related air pollution.
Health risks from extreme heat are growing, varying by population and geography
The risks of short- and long-term exposure to extreme heat are among the best-studied aspects of climate change. Emerging research has linked heat exposure to poor sleep quality, worse mental health, higher suicide rates, and increased crime rates – in addition to the multiple other threats it poses to health (see 2018 Brief).9_, 10_, 11_, 12_, 13_ More than a third of urban heat-related deaths in the 1990s and early 2000s can be attributed to climate change,14_ and climate change has further increased the frequency, duration, and intensity of heatwaves2_ since that time – putting more people at risk.
Vulnerability to extreme heat varies and more severe impacts can be seen in certain populations and regions of the country. Policy failures continue to disproportionately expose specific groups to extreme heat, such as outdoor workers, incarcerated persons, people of color, historically redlined communities (see 2020 Brief), and those living below the poverty line.15_, 16_, 17_ Age can increase susceptibility. In 2020, adults over the age of 65 experienced a total of nearly 300 million more days of heatwave exposure in the U.S. compared to the 1986-2005 average baseline, making it the second highest year of exposure recorded since 1986FN1, FN2, FN3.1_ Infants under one year experienced a total of nearly 22 million more days of heatwave exposure in 2020 with respect to that same baseline.
Factors like poorly designed infrastructure, limited access to air conditioning (A/C), and a lack of acclimatization can lead to heat-related harms occurring at lower-than-expected temperatures in historically cooler parts of the country. The typical peak of heat-related hospitalizations occurs at markedly lower heat indexesFN4 in the Northwest (80°F; 27°C) than the Southwest (100°F; 38°C).18_ Thus, communities in the Pacific Northwest (PNW) were at significantly increased risk when the unprecedented six days of excessive heat in June 2021 led to absolute temperatures up to 116°F (47°C) in cities such as Portland, Oregon.19_ The PNW heatwave was found to be “virtually impossible without human-caused climate change.”1_, 20_, 21_ Heat-related emergency department visits in the region were nearly 70 times higher than the same time period in 2019.22_ Media reports noted that the heatwave caused an estimated 600 deaths during one week in Washington and Oregon.23_
Droughts harm health broadly and worsen inequities, often in rural areas
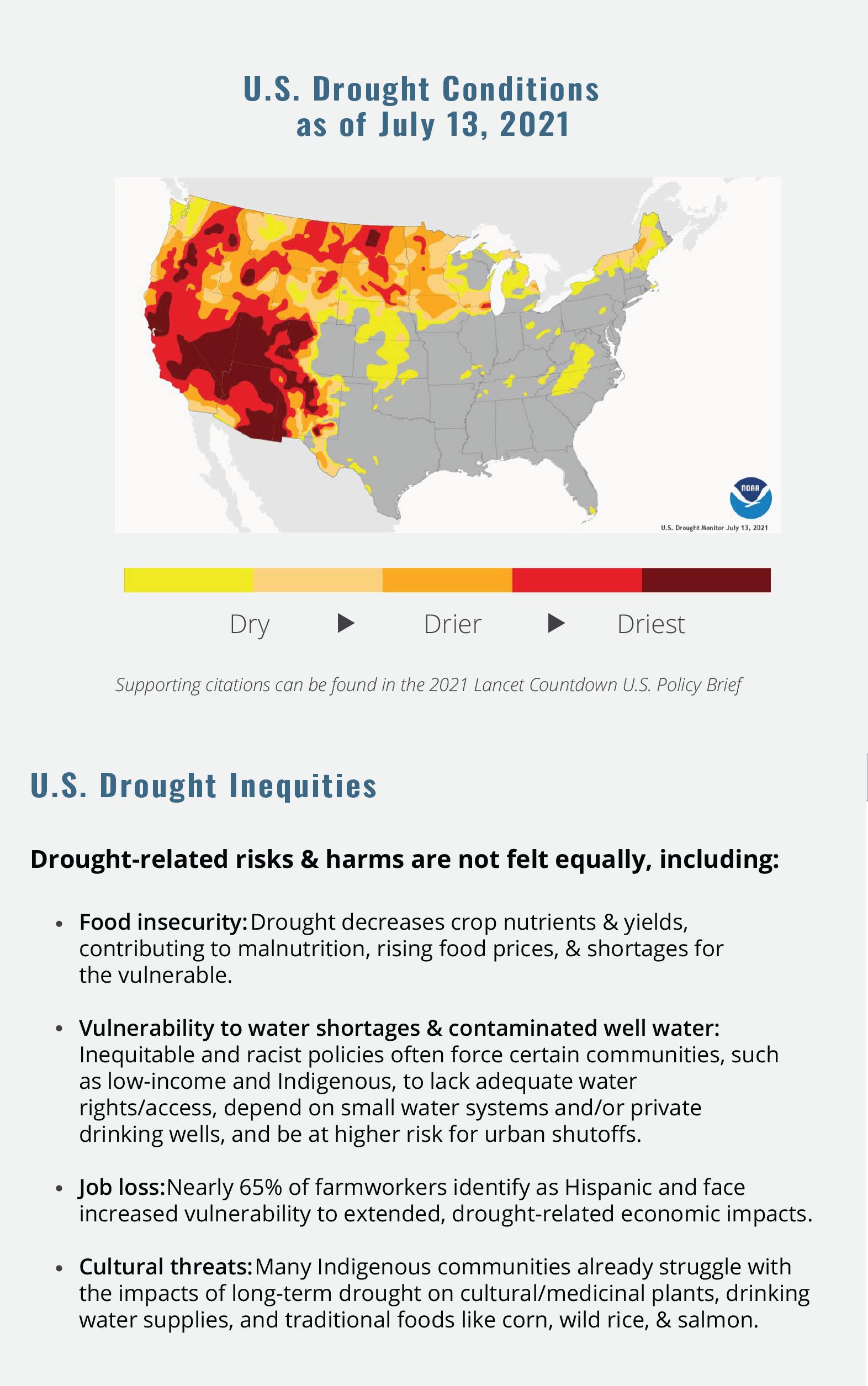
While definitions of drought vary, it is often defined as a water shortage that is not able to meet demand.24_ Drought has increased substantially across the Western and Central U.S. since 2020, with some areas facing the worst conditions in over a century.3_, 24_, 25_ As climate change is driving drought in much of the U.S., an understanding of the full breadth of associated health risks is essential to optimally prevent harm. Drought harms health in indirect and underrecognized ways by compounding exposure to heat, increasing risk of respiratory and infectious disease, worsening water quality, and exacerbating mental health issues, particularly in rural areas (see Figure 1).
Figure 1: Direct and indirect health impacts of drought in the U.S.
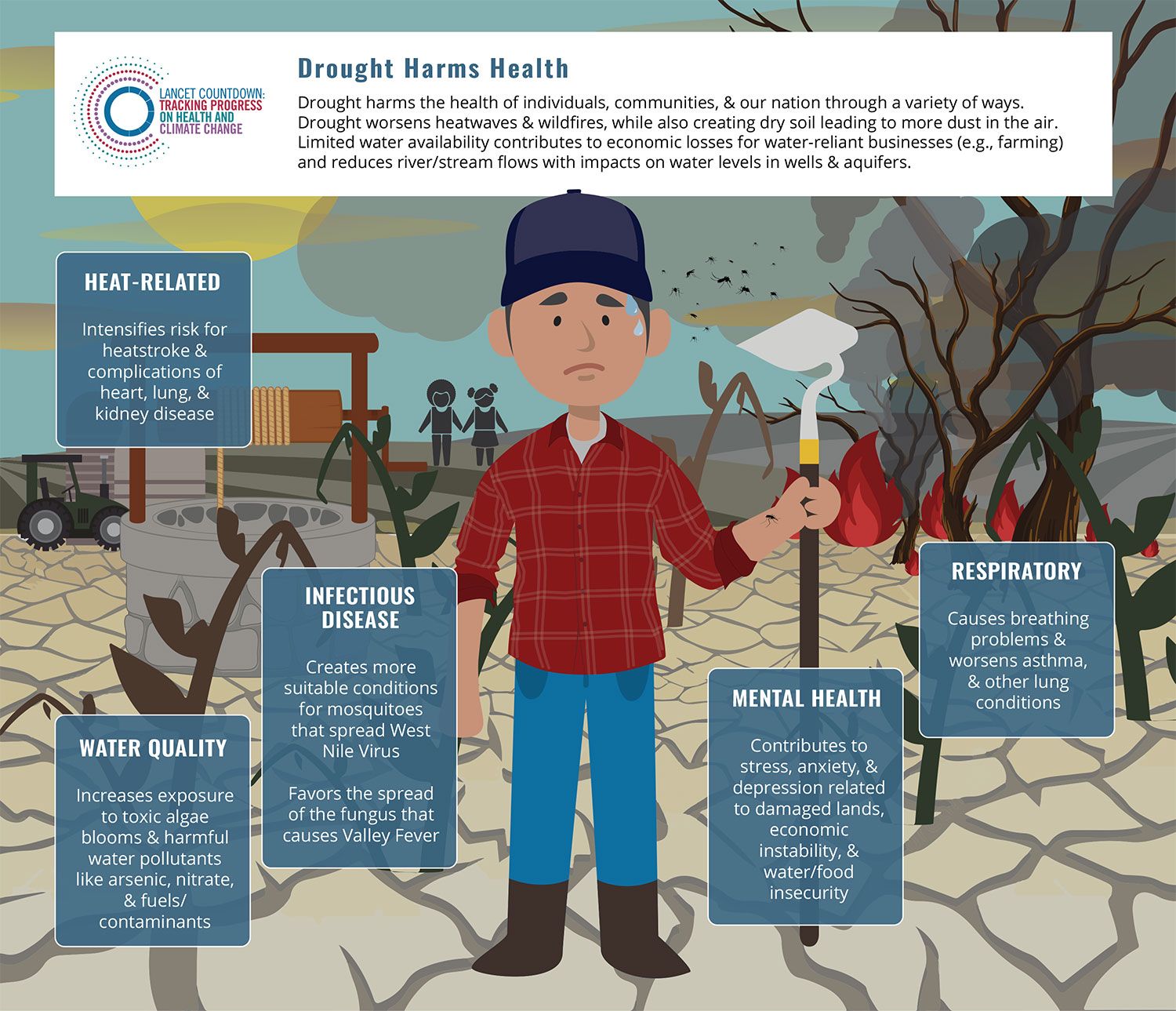
Infographic References26_, 27_, 28_, 29_, 30_, 31_, 32_, 33_, 34_, 35_, 36_, 37_, 38_
Health impacts of wildfires are also experienced far from the event
Extreme heat combined with extended drought conditions triggered a record-breaking wildfire season in the Western U.S. in 2020,2_, 39_ a trend that has continued in 2021. Wildfires in the Western U.S. are associated with hotter temperatures, and the wildfire season has been lengthening. In the time series depicted in Figure 2, by September 2020 the maximum annual wildfire incidence peaked at approximately 80,000 wildfires, 8 times greater than the total incidence in 2001 FN5.
Figure 2: Cumulative annual wildfire incidence by month in the Western U.S., 2001-2020, with annual temperature anomalies.
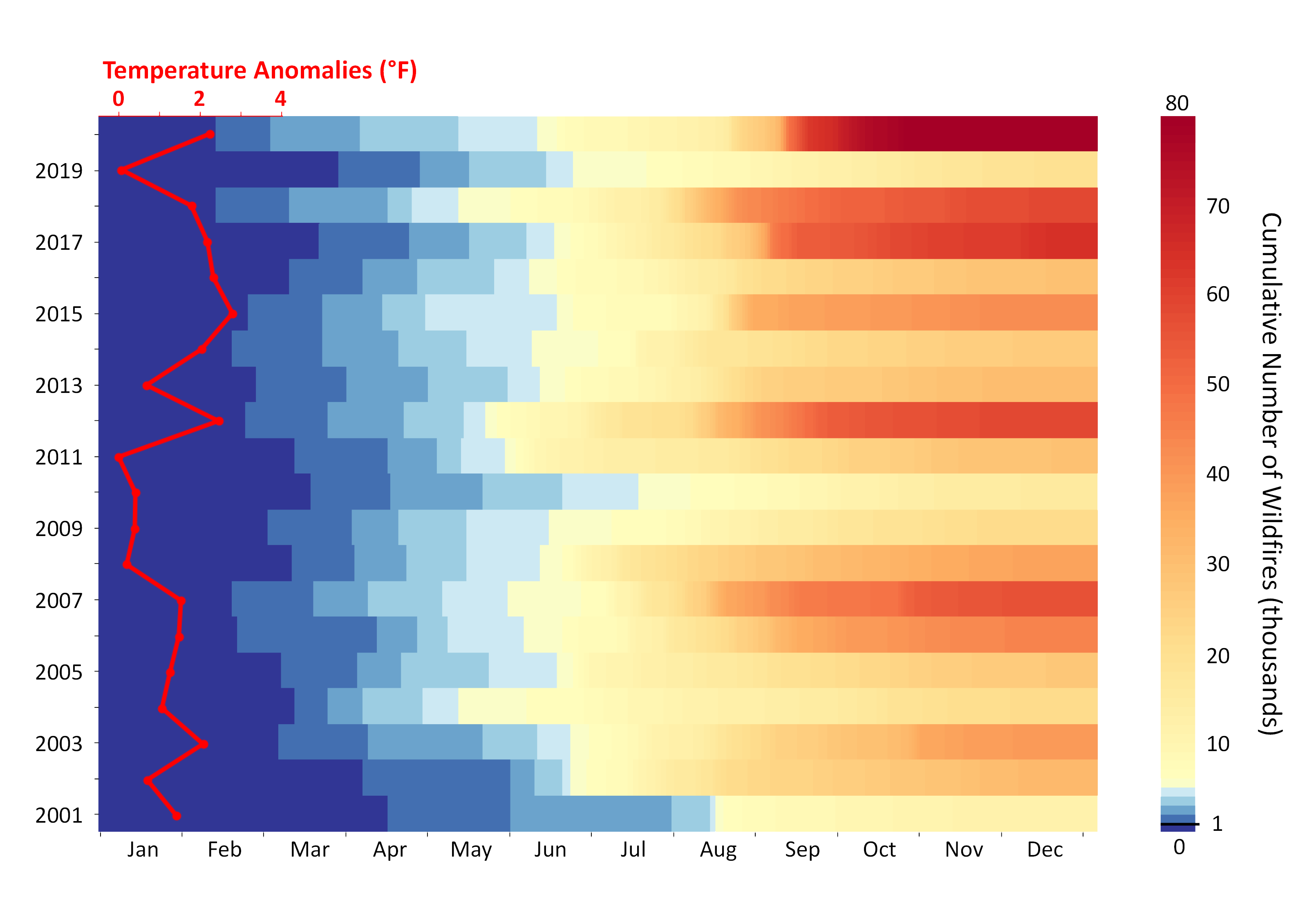
The figure depicts daily cumulative presumed vegetation wildfires at nominal and high confidence levels (confidence ≥ 30%) in the western U.S. (Arizona, California, Colorado, Idaho, Montana, Nevada, New Mexico, Oregon, Utah, Washington, and Wyoming) from 2001 to 2020. As depicted, cumulative fire incidence reached 1,000 (midweight blue) by early April during the early 2000s (e.g., 2001, 2002); notably, that same cumulative incidence tended to be reached by early February during the late 2010s (e.g., 2018, 2020). The baseline period for temperature is 1980-2000. Note: Each fire was counted as an Infrared thermal anomaly detectable in a 1-km2_ pixel. Temperature data derived from NASA Daymet and wildfire data from NASA MODIS/Aqua+Terra Thermal Anomalies/Fire locations product.FN5
Wildfire smoke contains numerous harmful air pollutants, such as particulate matter (PM), carbon monoxide, and precursors (e.g., nitrogen oxides, volatile organic compounds) that generate ground-level ozone in the presence of heat and sunlight.40_ There is emerging evidence that wildfire-related fine PM, or PM2.5, from wildfire smoke may be up to 10 times more harmful to human health than PM2.5 from other sources,41_ with increased respiratory harms for children.42_ Exposure to wildfire smoke is associated with an increased risk of heart and lung disease, an increase in premature death,43_, 44_ worsened mental health,45_ and greater risk of preterm birth.46_
While some of the most damaging wildfires occur in the Western U.S., their health effects are felt across the country. Wildfire smoke contributed 25% of total PM2.5 exposure across the continental U.S., and up to 50% in the Western U.S. in 2016-2018 compared to less than 20% a decade ago.47_ Between 1997-2016, wildfires also increased the number of eight-hour periods with unhealthy ground-level ozone levels by about 10%, and many regions would not have had these levels without the presence of wildfiresFN6.48_
Worsening air quality has been observed thousands of miles downwind from the origin of the fire. In July 2021, wildfire smoke from California’s massive Dixie Fire reached as far east as Maine, impacting air quality in states throughout the East Coast and contributing to the worst air quality in New York City in 15 years.49_, 50_, 51_ During the 2020 California wildfires, PM2.5 levels were upwards of 14 times the current health-based limitFN7 in the vicinity of the wildfires and four times the limit over 600 miles away.40_ Early evidence also suggests that smoke-related health impacts may be greater farther away from the origin of the fire. This could be due, in part, to smoke becoming more toxic over time through a process called oxidation, as well as people not recognizing the dangerous air quality and failing to change their behavior.40_, 52_, 53_
A variety of factors, such as restricted access to resources, poverty, and forced concentration of marginalized communities in high-risk areas due to discriminatory housing policies, place certain communities at increased risk. For example, Black, Latinx, and American Indian families, as well as low-income communities and incarcerated persons in wildland firefighting programs, are at greater risk for health harms from wildfires.40_,54_, 55_, 56_, 57_, 58_, 59_ A better understanding of these inequities is critical because disease and death from wildfire smoke exposure are projected to continue to grow as wildfires worsen.2_, 43_
Critical Insight:
Climate change is already influencing the spread of infectious diseases regularly found in the U.S. For example, longer warm seasons over a larger geographic area have contributed to an increased incidence of Lyme disease,60_ which is spread through two tick species (Ixodes scapularis and I. pacificus). Climate change may also influence the spread of new infectious diseases in the U.S., including the transmission potential (R0) determining how likely one infection is to lead to another. Dengue is a potentially deadly mosquito-borne viral infection with cases increasing globally.1_ Current dengue cases in the U.S. are largely related to foreign travel.61_ However as a result of changes in temperature, rainfall and humidity, environmental conditions have become increasingly suitable for the spread of dengue through Aedes aegypti mosquitoes in the U.S. since the 1950sFN8.1_ In the past 5 years (2016-2020), the transmission potential was on average 55.6% higher than in baseline years (1950-1954), and briefly rose above the key threshold of one for the first time in 2017. A transmission potential above one means that one case of dengue can cause more than one additional infection, potentially leading to an outbreak in the right conditions.
Critical Insight:
Climate change makes existing problems worse as climate-linked events interact with other stressors to threaten lives, undermine population health, and stress health systems. This concept of threat multiplication has been shown throughout the COVID-19 pandemic, but it is especially of concern as the U.S. faces renewed challenges posed by variants. Climate-intensified events, such as extreme heat and hurricanes, can threaten key components of pandemic mitigation strategies such as social distancing and reduced mobility.62_, 63_ Furthermore, PM from climate-intensified wildfire smoke has been associated with an increased susceptibility of contracting and dying from COVID-19.64_ This association is thought to result from PM enabling virus transport over greater distances and causing more lung inflammation, increasing the risk of severe disease.65_, 66_, 67_
The pandemic has revealed critical capacity shortages in the U.S. healthcare system and supply and demand mismatches,68_ particularly in emergency and critical care systems and rural healthcare.65_, 66_, 69_
Staff, equipment (e.g., ventilators), and supply chain shortages (e.g., personal protective equipment) throughout the pandemic have strained health systems across the country with implications for all who seek care. Overwhelmed systems provide compromised care, at least intermittently,70_ that is often inequitable.71_, 72_ For example, some U.S. locales have been forced to adopt crisis standards of care, which is when state governments declare a change in normal health system operations and care due to a pervasive or catastrophic event.73_
Throughout the pandemic, infrastructure damage, power outages, and increased care needs have exacerbated the impact of climate-fueled extreme weather events (e.g., wildfires, floods, hurricanes and extreme heat) on overwhelmed systems. As a result, cascading failures have underscored the structural weakness of our interconnected systems and failure to manage the extreme challenges posed by compounding crises. As climate change continues to increase the likelihood of compound hazards, these capacity challenges will likely become more frequent, widespread, and consequential for all health conditions. Updating disaster planning scenarios to include compound events, conducting health system stress tests to discern limits and identify where systems are likely to be seriously constrained, and ensuring health systems are climate-resilient are potential strategies to limit the impacts of these events when they occur.74_, 75_
Evidence-Informed Policy Recommendations that Prioritize Health and Equity
Policy needs to be guided by an understanding of how climate change inequitably harms health. The Brief outlines policy recommendations in three key focus areas: 1) Adaptation, or interventions that protect health, 2) Economics & Finance, and 3) Mitigation, or efforts to reduce emissions to slow climate change. The reduction of inequities can benefit health and society broadly,76_ and these recommendations highlight how health and equity can serve as guiding principles in the response to climate change.
 Adaptation: Rapidly increase funding for health protections: Local, climate-specific health research conducted through multi-sectoral partnerships can directly inform the development, implementation, and evaluation of equitable health-protective actions.
Adaptation: Rapidly increase funding for health protections: Local, climate-specific health research conducted through multi-sectoral partnerships can directly inform the development, implementation, and evaluation of equitable health-protective actions.
 Economics & Finance: Incorporate health-related costs of fossil fuels into the social cost of carbon: U.S. calculations must include these health-related costs to accurately analyze the costs and benefits of policies that contribute to the release of carbon dioxide.
Economics & Finance: Incorporate health-related costs of fossil fuels into the social cost of carbon: U.S. calculations must include these health-related costs to accurately analyze the costs and benefits of policies that contribute to the release of carbon dioxide.
 Mitigation: Urgent and equitable economy-wide GHG emission reductions: Rapidly reduce economy-wide GHG emissions to 57-63% of 2005 levels by 2030, consistent with a 1.5°C national emissions pathway, and a near zero-emission economy by mid-century. Direct at least 40% of investments directed towards improving air quality in under-resourced communities.
Mitigation: Urgent and equitable economy-wide GHG emission reductions: Rapidly reduce economy-wide GHG emissions to 57-63% of 2005 levels by 2030, consistent with a 1.5°C national emissions pathway, and a near zero-emission economy by mid-century. Direct at least 40% of investments directed towards improving air quality in under-resourced communities.
Adaptation
Evidence-informed implementation of protective actions is essential to improve health and equity: Air conditioning as an example
Even with rapid reductions in GHGs, the U.S. will increasingly experience health harms like those outlined. Inequitable policies and practices systematically restrict equitable access to climate-resilient resources and infrastructure. It is imperative that an understanding of health risks and inequities guide actions to adapt and implement health protections. A/C, for example, is a vital but flawed health protection, as it contributes to GHG emissions and air pollution. In addition, access to A/C varies by region, is unreliable due to factors like power outages, and is inequitable because of associated expenses (e.g., electricity costs). These limitations necessitate a multi-pronged, evidence-informed policy approach to health protections from extreme heat.
In 2019, A/C was estimated to prevent approximately 48,000 heat-related deaths in the U.S. in those over the age of 65FN9.1_ In addition, access to A/C in the U.S. has increased by 11% since 2000 to include about 92% of households in 2019.1_ However, access varies significantly, and is more limited in historically cooler regions. Nearly 30% of households lack access to A/C in the Pacific region; Seattle, Washington is one of the least air-conditioned cities with 56% of households lacking access,77_ providing further context to the regional variation in heat-related illness and death and the mass casualties from the PNW heatwave in June 2021. Access also does not always mean that households are able to effectively operate A/C due to factors like rotating power outages during times of peak demand78_ or outages from extreme weather events.79_
Electricity costs are additional barriers for many, exacerbated by inequitable policies.80_, 81, 82_ For example, in the U.S., energy cost disparities are higher for Black and Latinx households compared to non-Hispanic white households, and a lack of access to affordable, renewable energy puts Black households at disproportionate risk.81_, 83_, 84_, 85_, 86_ Additionally, inequitable access to weatherized, energy-efficient homes limits adaptability for low-income communities and people of color.87_, 88_
These issues have life and death consequences. In 2020, Arizona experienced record-breaking heat and a record 522 heat-related deaths, 89_ which was nearly three times the yearly baseline average in the first half of the previous decade.FN10 Maricopa County accounted for 323 of those deaths, almost a five-fold increase above the 2000-2014 baseline average.90_ More than half of those individuals were without housing, over 60% were 50 years and older, and Black and Indigenous people had the highest rates of deaths — mirroring national trends.90_, 91_ Over 80% of persons suffering an indoor heat-related death in 2020 had an A/C unit present within their building, but two-thirds of the units were not functioning and one-third were not running.90_, 92_
Lastly, the energy used for A/C is largely derived from the burning of fossil fuels. Thus, the use of A/C contributed to an estimated 500 additional deaths from air pollution exposure and worsened climate change by emitting over 260 megatonnes of carbon dioxide in 2019FN10.1_
These flaws show us that A/C as a primary health protective strategy from heat is currently insufficient, and the complexities mandate a multi-pronged response guided by an evidence-informed understanding of the inequitable health risks. This understanding must occur at a variety of levels (e.g., individual, building, neighborhood) to develop, implement, evaluate, monitor, and communicate the most effective, sustainable health protections.93_ Many policy solutions exist for extreme heat that can act at these different levels, such as well-communicated action plans for the individual,94_, 95_ tax incentives or rebates for green building codes and sustainable energy solutions, equitable implementation of interventions like cooling technologies such as heat pumps,96_ home retrofits and weatherization,97_ cool roofs98_ for buildings, and increased greenspace and water bodies in urban environments (e.g., tree planting, fountains) for neighborhoods.93_, 99_ During this transition to multi-pronged, sustainable approaches, numerous policy options can serve as a bridge. These may include the use of A/C vouchers, geothermal and solar tax incentives or rebates to power A/C, eliminating electricity surge pricing, creating moratoria on power shut offs, and ensuring equitable access to cooling centers. Collectively, these types of interventions can protect health, improve equity, and increase our resilience to extreme heat events.
More generally, health must be a driver for proactive preventive planning, whether for local heat-health protection plans or reducing risks from other aspects of climate change. This includes integrating the health perspective into multi-sectoral policy discussions.
The Biden-Harris administration created the Office of Climate Change and Health Equity within the U.S. Department of Health and Human Services to identify and coordinate with communities who face inequitable climate vulnerabilities.100_ While an encouraging start, enormous opportunities remain.
Economics & Finance
The health-related costs of fossil fuel use are substantial and must be factored into fiscal analyses and decision-making across all levels and sectors
Economic signals are powerful motivators for social change and governmental action. Given that the health of everyone is impacted to some degree by the extraction and use of fossil fuels – from climate change to air pollution – ignoring health-related costs leads to a flawed and narrow understanding of the economic benefits of action on climate change.
The totality of the health-related societal costs of fossil fuels, such as higher out-of-pocket health expenses, lost wages, and loss of life or quality of life, are not fully known and largely unmeasured. Estimates for fossil fuel-related air pollution are increasingly available, such as attributable deaths, and what is currently known suggests the health-related costs of air pollution are substantial101_ with differences found locally.102_
The continued burning of fossil fuels drives climate change-related health harms, the costs of which are on the order of billions to trillions annually just for one type of health harm (e.g., heat-related deaths) or event (e.g., one hurricane).103_, 104_ The 2018 California wildfires caused an estimated $32 billion dollars in health costsFN11, over half of which were outside California.105_ These costs are predicted to increase significantly. Reductions in GHG emissions would result in health benefits from improved air quality that alone may be comparable to or exceed the costs of control.106_, 107_, 108_, 109_
The social cost of carbon (SCC) attempts to quantify the costs of future harm caused by the release of one additional ton of carbon dioxide. Incorporating the full breadth of costs associated with climate-related deaths and illness would substantially increase the SCC.103_, 110_, 111_ Other GHGs, including methane and nitrous oxide, also have associated health harms (see 2020 Brief). An Executive Order created an Interagency Working Group on the Social Cost of GHGs, which expands beyond SCC to also include the social cost of methane (SCM) and the social cost of nitrous oxide (SCN).112_ Updated SCC, SCM, and SCN are to be released by January 2022. While human health is listed as one of the included factors, further research is needed to achieve a full understanding of the health-related costs of GHGs. Thus, accounting for the additional GHG-driven costs of health harms is fundamental113_ and will dramatically alter the calculations. This further reinforces that a rapid and swift transition away from fossil fuels improves health and equity and is cost effective.
Mitigation
Health and equity benefits should motivate and guide a swift transition to a zero-emission economy
Urgent economy-wide reductions in GHG emissions must be consistent with a national emissions pathway that limits the global average temperature rise to 1.5°C, currently estimated to be a 57-63% reduction from 2005 levels of U.S. emissions, by 2030.114_ The faster an equitable transition away from fossil fuels occurs, the greater the health benefits.2_, 115_ This includes a reduction in air pollution-related deaths and disease, and decreased climate change-related health harms and health system impacts.109_, 115_ It is critical to recognize that these transitions also represent a tremendous opportunity to correct existing inequities and environmental injustices.116_, 117_ Importantly, benefits would go beyond national borders. According to the 2021 global report of the Lancet Countdown, the U.S. contributed 15% of global GHG emissions from the burning of fossil fuels in 2019FN12.1_
Decades of racially-biased policies — both implicit and explicit — including structural discrimination in housing, zoning, and the placement of industrial and transportation infrastructure have resulted in widespread and persistent air pollution inequities.118_ Across the majority of states, exposure to air pollution is higher for Black, Latinx, Alaskan Native or American Indian, Asian American or Pacific Islander, and other people of color, even when controlling for income, in nearly every emissions category in rural and urban areas.119_ Policies to cut GHG emissions should focus most immediately on transitioning away from high-polluting fossil-fuel infrastructure in and adjacent to low-income communities and those most impacted.
While GHG reductions need to occur across the entire U.S. economy, the electricity generation and transportation sectors are major focuses as they contributed to over half of the U.S. GHG emissions in 2019, at 25% and 29%, respectively.120_ For electricity generation, coal remains the largest and most polluting source for both GHGs and air pollution. Although coal use has been reduced by about half since 2007, it was still responsible for about 19% of all electricity generation in 2020.121_ While renewable energy — mainly wind, hydropower, and solar — have grown rapidly and account for about 20% of electricity, natural gas is now 40% and biomass is 1.4%.121_ Reductions can also stem from increasing efficiency and managing demand. As coal use decreases, negative health impacts from coal combustion are in decline, but the harms from burning natural gas (see 2020 Brief) and biomass are on the rise.122_ Continued investments in fossil fuel infrastructure and extraction is locking in emissions for decades and putting the 1.5°C limit out of reach,123_, 124_ and our lagging transition to zero-emission energy is harming health inequitably.
Within the transportation sector, petroleum products (e.g., gasoline) made up more than 90% of energy or fuel sources in 2020, while electricity was less than 1%.125_ Though alternatives to passenger vehicles, like walking and biking, have health benefits109_, they aren’t the sole solution. Even a 50% drop in passenger vehicle traffic wasn’t enough to erase disparities in traffic-related air pollution during the COVID-19 pandemic.126_ Further, these alternatives are not equally feasible across all communities. Similarly, while a transition to a zero-emission transportation sector needs to be a part of the effort to curb GHG emissions, factors such as electricity sources and availability of charging stations must be considered to avoid leaving lower-income and rural communities behind and worsening health disparities.127_
The Biden-Harris administration has committed to an economy-wide GHG emissions reduction of 50-52% by 2030 from 2005 levels,128_, 129_ 100% carbon pollution free electricity by 2035,128_ and to ensure that at least 40% of the benefits from climate and clean energy investments benefit under-resourced communities.130_ If they succeed, these are important steps in the right direction, but much more is required to optimally protect health and advance equity.
Organizations and acknowledgements
U.S. Brief Authors: Renee N. Salas, MD, MPH, MS; Paige Knappenberger Lester, MA; Jeremy J. Hess, MD, MPH
Additional Team Acknowledgements: Support, Logistics, & Review: Carissa Novak, MScGH; Vivian Taylor, MPP, MDiv; Luke Testa; Toochi Uradu. Executive Summary Lead: Naomi Beyeler, MPH, MCP. Figure 1 Infographic Designer: Mina Lee, MPA. Figure 2: Yun Hang, MS, PhD; Yang Liu, PhD. Copy Editing & References: James Healy, MPH; Laura E. Peterson, BSN, SM; Katharine Poole, MA. Spanish Translation and Copy Editing: Juan Aguilera, MD, PhD, MPH. Website & Summary PDF Design: D’lynne Plummer and team.
Review on Behalf of the Lancet Countdown (alphabetical): Anthony Costello, FmedSCi; Frances MacGuire, PhD, MPH; Marina Romanello, PhD; Ian Hamilton, PhD.
Review on Behalf of the American Public Health Association (alphabetical): Ivana Castellanos, MPH; Evelyn Maldonado, BS; Katherine Robb, MSPH; Tia Williams, MPH, CNS.
Science and Technical Advisors (alphabetical): These science and technical advisors provided technical and review assistance but are not responsible for the content of the report, and this report does not represent the views of their respective federal institutions. Caitlin A. Gould, MPPA, DrPH (ABD); Rhonda J. Moore, PhD; Ambarish Vaidyanathan, PhD.
Working Group Reviewers of Brief and/or Executive Summaries for Target Audiences (alphabetical): Ploy Achakulwisut, PhD; Susan Anenberg, MS, PhD; Mona Arora, PhD, MSPH; Jesse E. Bell, PhD; Aaron Bernstein, MD, MPH; Naomi Beyeler, MPH, MCP; Erin Biehl, MSPH; Laura Bozzi, PhD; Robert Bryon, MD, MPH; Juanita Constible, MSc; Cara Cook, MS, RN, AHN-BC; Natasha DeJarnett, PhD, MPH; Michael A. Diefenbach, PhD; Caleb Dresser, MD, MPH; Kristie Ebi, PhD, MPH; Matthew Eckelman, PhD; Luis E. Escobar DVM, PhD; Sarah Fackler, MA; Meghana Gadgil, MD, MPH, FACP; Ilyssa O. Gordon, MD, PhD; Chelsea L. Gridley-Smith, PhD; Adrienne Hollis, PhD, JD; J. Harry Isaacson, MD; Patrick Kinney, ScD, MS; Philip J. Landrigan, MD, MSc, FAAP; Rachel Lookadoo, JD; Melissa C. Lott, PhD; Yang Liu, PhD; Edward Maibach, PhD, MPH; Leyla Erk McCurdy, MPhil; Anna Miller, MPH; Nick Obradovich, PhD; Jacqueline Patterson, MSW, MPH; Lisa Patel, MD, MESc; Jonathan Patz, MD, MPH; Rebecca Philipsborn, MD, MPA; Stephen Posner, PhD; Liz Purchia; Rebecca Rehr, MPH; Caitlin Rublee, MD, MPH; Heidi Honegger Rogers DNP, FNP-C, APHN-BC; Robyn Kaplan Rothman, JD; Ananya Roy, Sc.D; Mona Sarfaty, MD, MPH; Liz Scott; Emily Senay, MD, MPH; Jeffrey Shaman, PhD; Jodi D. Sherman, MD; Cecilia Sorensen, MD; Sarah Spengeman, PhD; Vishnu Laalitha Surapaneni, MD, MPH; Jon Utech, MBA, MPOD; J. Jason West, MS, MPhil, PhD; Kristi E. White, PhD, ABPP; Carol C. Ziegler, APRN, NP-C, AHNP-BC; Lewis H. Ziska, PhD.
THE LANCET COUNTDOWN
The Lancet Countdown: Tracking Progress on Health and Climate Change is an international, multi-disciplinary collaboration that exists to monitor the links between public health and climate change. It brings together 38 academic institutions and United Nations agencies from every continent, drawing on the expertise of climate scientists, engineers, economists, political scientists, public health professionals, and doctors. Each year, the Lancet Countdown publishes an annual assessment of the state of climate change and human health, seeking to provide decision-makers with access to high-quality evidence-based policy guidance. For the full 2021 assessment, visit www.lancetcountdown.org/2021-report/.
THE AMERICAN PUBLIC HEALTH ASSOCIATION
The American Public Health Association (APHA) champions the health of all people and all communities. It strengthens the public health profession, promotes best practices, and shares the latest public health research and information. The APHA is the only organization that influences federal policy, has a nearly 150-year perspective, and brings together members from all fields of public health. In 2018, APHA also launched the Center for Climate, Health and Equity. With a long-standing commitment to climate as a health issue, APHA’s Center applies principles of health equity to help shape climate policy, engagement, and action to justly address the needs of all communities regardless of age, geography, race, income, gender and more. APHA is the leading voice on the connection between climate and public health. Learn more at www.apha.org/climate.
Recommended Citation: Lancet Countdown, 2021: 2021 Lancet Countdown on Health and Climate Change Policy Brief for the United States of America. Salas RN, Lester PK, Hess JJ. Lancet Countdown U.S. Policy Brief, London, United Kingdom.
Climate change & health in U.S.Extreme heat – Growing & varyingDroughts – Broad health harmsFIGURE 1: Drought health harms & inequitiesWildfires – Faraway health harmsFIGURE 2: Cumulative annual wildfire incidenceResearch helps anticipate growing threatsClimate change & health system capacityEvidence-informed policy recommendations – Adaptation – Air conditioning as an example – Economics – Factoring in health costs & Finance – Mitigation – Health & equity benefits as a guideAcknowledgements